Hydroxychloroquine¶
Fig. 5 Hydroxychloroquine¶
‘Only a one in 17 billion chance hydroxychloroquine doesn’t work’: medical professor Source: [skynews.com.au, November 29 2020 : ‘Only a one in 17 billion chance hydroxychloroquine doesn’t work’: medical professor](https://www.skynews.com.au/details/_6212859932001?fbclid=IwAR0Qzx3BAeJtPoqN958ZFnc3ckUdfQlEr0zuIly69-Gl-mJ3cmPPmcfRjrE)
Hydroxychloroquine really works says Professor of Medicine Dr Peter McCullough, describing the treatment as “the most widely used therapeutic” to treat COVID-19 in the world.
“The chances that it doesn’t work are calculated to be one in 17 billion,” he told Sky News.
“There’s no controversy over whether or not hydroxychloroquine works. The controversy is on the public health approach to COVID-19.”
Mr McCullough said “the virus invades inside cells, so we have to use drugs that go inside the cell and work to reduce viral replication”.
“The drugs that work within the cell and actually reduce viral replication are hydroxychloroquine, Ivermectin, doxycycline and azithromycin”.
“Sadly, in the United States and I know in Australia this happens all the time, patients get no treatment whatsoever. They literally are told to stay at home until they are sick enough to go to the hospital”
“I think that honestly it’s atrocious.
“History will look back on that and think it was the worst way to handle a potentially fatal illness.”
Common uses of Hydroxychloroquine¶
Hydroxychloroquine has long been commonly used to treat Rheumatoid arthritis and Lupus
Additional Studies and Reports about Hydroxychloroquine¶
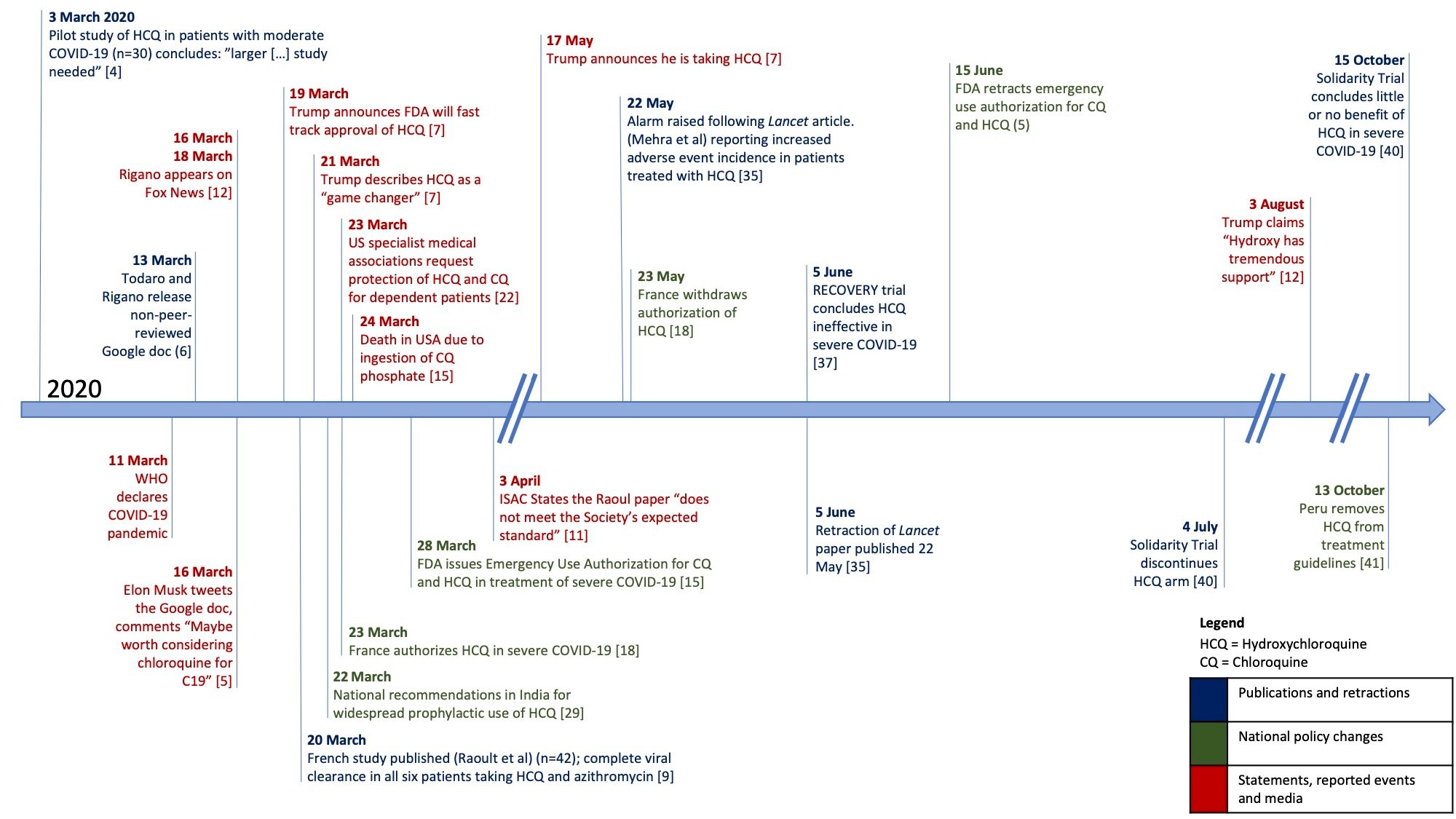
Fig. 6 Timeline of key events in the story of chloroquine/hydroxychloroquine and COVID‐19¶
“Contested effects and chaotic policies: the 2020 story of (hydroxy) chloroquine for treating COVID‐19” [Cochrane Library]. • Handy timeline:
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.ED000151/full
antiviral activity Phospholipidosis appears enhanced by cationic amphiphilic drugs including Hydroxychloroquine and Azithromycin¶
Phospholipidosis is a shared mechanism underlying the in vitro antiviral activity of many repurposed drugs against SARS-CoV-2
Tia A. Tummino, Veronica V. Rezelj, Benoit Fischer, Audrey Fischer, Matthew J. O’Meara, Blandine Monel, Thomas Vallet, Ziyang Zhang, Assaf Alon, Henry R. O’Donnell, Jiankun Lyu, Heiko Schadt, Kris M White, Nevan J. Krogan, Laszlo Urban, Kevan M. Shokat, Andrew C. Kruse, Adolfo García-Sastre, Olivier Schwartz, Francesca Moretti, Marco Vignuzzi, Francois Pognan, Brian K. Shoichet
bioRxiv 2021.03.23.436648; doi: https://doi.org/10.1101/2021.03.23.436648
“Phospholipidosis is a shared mechanism underlying the in vitro antiviral activity of many repurposed drugs against SARS-CoV-2” (preprint) [bioRxiv].
“Repurposing drugs as treatments for COVID-19 has drawn much attention. A common strategy has been to screen for established drugs, typically developed for other indications, that are antiviral in cells or organisms. Intriguingly, most of the drugs that have emerged from these campaigns, though diverse in structure, share a common physical property: cationic amphiphilicity. Provoked by the similarity of these repurposed drugs to those inducing phospholipidosis, a well-known drug side effect, we investigated phospholipidosis as a mechanism for antiviral activity. We tested 23 cationic amphiphilic drugs—including those from phenotypic screens and others that we ourselves had found—for induction of phospholipidosis in cell culture. We found that most of the repurposed drugs, which included hydroxychloroquine, azithromycin, amiodarone, and four others that have already progressed to clinical trials, induced phospholipidosis in the same concentration range as their antiviral activity; indeed, there was a strong monotonic correlation between antiviral efficacy and the magnitude of the phospholipidosis. Conversely, drugs active against the same targets that did not induce phospholipidosis were not antiviral.”
cationic amphiphilicity. Provoked by the similarity of these repurposed drugs to those inducing phospholipidosis, a well-known drug side effect, we investigated phospholipidosis as a mechanism for antiviral activity. We tested 23 cationic amphiphilic drugs—including those from phenotypic screens and others that we ourselves had found—for induction of phospholipidosis in cell culture. We found that most of the repurposed drugs, which included hydroxychloroquine, azithromycin, amiodarone, and four others that have already progressed to clinical trials, induced phospholipidosis in the same concentration range as their antiviral activity; indeed, there was a strong monotonic correlation between antiviral efficacy and the magnitude of the phospholipidosis. Conversely, drugs active against the same targets that did not induce phospholipidosis were not antiviral.”
https://www.biorxiv.org/content/10.1101/2021.03.23.436648v1
Last change: Tue, 03 Aug 2021 10:25 PM UTC